News
-
17 February 2014
"Vita" hospital performs innovative surgic... -
13 May 2013
FREE ORTHOPAEDIC EXAMINATIONS AT ‘VITA’ -
03 September 2012
Injuries from motorcycle accidents fill th... -
11 May 2012
Surgeons from "Vita" operated successfully... -
11 March 2009
Specialized NUCLEAR MAGNET RESONANCE for d...
|
Knee Arthroscopy 21.06.2013 Dr. Chanko Chankov
|
|
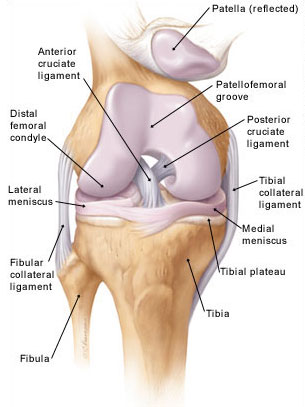
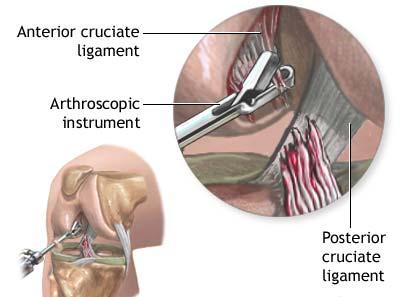
Anatomy of the knee joint The knee is the largest joint in the body. The knee joint is made up of the femur, tibia and patella (knee cap). All these bones are lined with articular (surface cartilage). This articular cartilage acts like a shock absorber and allows a smooth low friction surface for the knee to move on. Between the tibia and femur lie two floating cartilages called menisci. The medial (inner) meniscus and the Lateral (outer) meniscus rest on the tibial surface cartilage and are mobile. The menisci also act as shock absorbers and stabilizers. The knee is stabilized by ligaments that are both in and outside the joint. The medial and lateral collateral ligaments support the knee from excessive side-to-side movement. The (internal) anterior and posterior cruciate ligaments support the knee from buckling and giving way. The knee joint is surrounded by a capsule (envelope) that produces a small amount of synovial (lubrication) fluid to help with smooth motion. Thigh muscles are important secondary knee stabilizers.
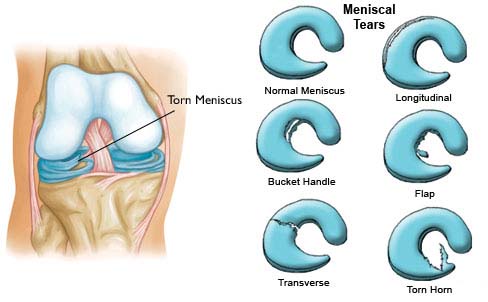
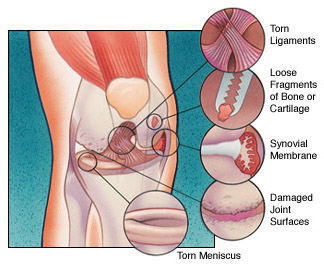
Menisci are located between the two major bones in the knee joint. Thy are internal and external and have the form of a disc-shaped crescent. The inner is large grown with the joint capsule and tibia and the outer is a small and free grown only with the tibia. Menisci take 60% of the load in the knee joint, reducing the working area of the cartilage at the point where the load is transmitted between the two major bones. They improve the stability of the joint in all its movements. About knee arthroscopy You may have knee arthroscopy to investigate problems such as inflammation or injury, or to repair damaged tissue and cartilage. It’s also used to take small tissue samples (biopsies), which can help to diagnose problems such as infection. Arthroscopy is useful in evaluating and treating the following conditions: 1. Torn floating cartilage (meniscus): The cartilage is trimmed to a stable rim or occasionally repaired
2. Torn surface (articular) cartilage
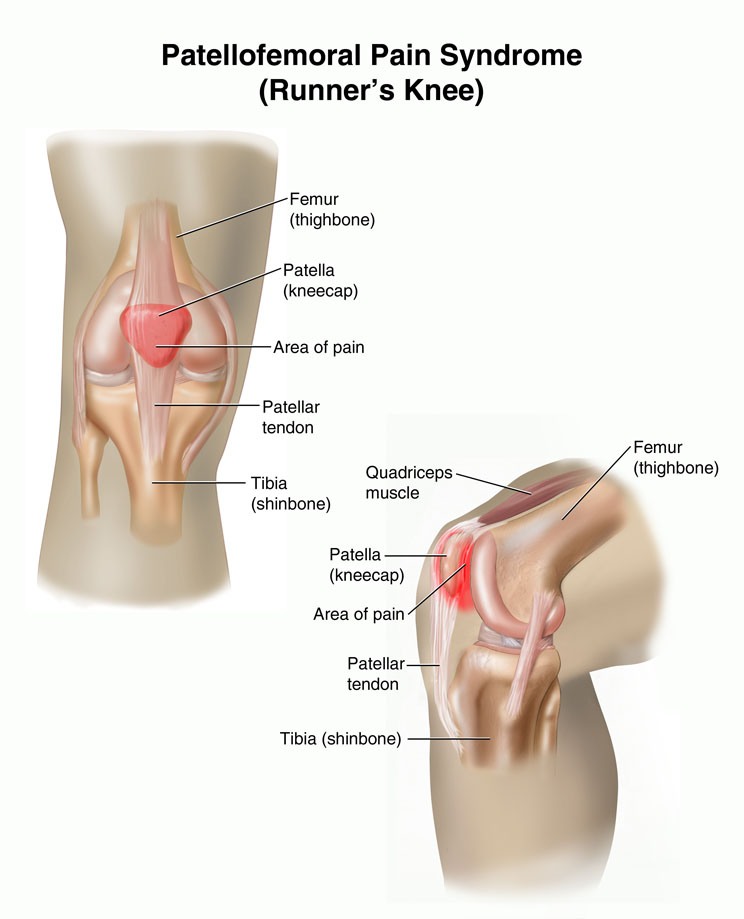
3. Removal of loose bodies (cartilage or bone that has broken off) and cysts. 4. Reconstruction of the Anterior Cruciate ligament 5. Patello-femoral (knee-cap) disorders
6. Washout of infected knees 7. General diagnostic purposes
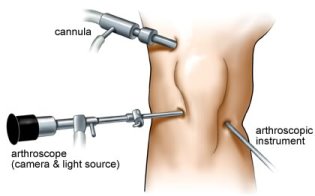
Before the Procedure Always tell your doctor or nurse what drugs you are taking, even drugs, supplements, or herbs you bought without a prescription. During the 2 weeks before your surgery: •You may be asked to stop taking drugs that make it harder for your blood to clot. These include aspirin, ibuprofen (Advil, Motrin), naproxen (Naprosyn, Aleve), and other drugs. •Ask your doctor which drugs you should still take on the day of your surgery. •Tell your doctor if you have been drinking a lot of alcohol, more than 1 or 2 drinks a day. •If you smoke, try to stop. Ask your doctor for help. Smoking can slow down wound and bone healing. •Always let your doctor know about any cold, flu, fever, herpes breakout, or other illness you may have before your surgery. On the day of your surgery: •You will usually be asked not to drink or eat anything for 6 to 12 hours before the procedure. •Take your drugs your doctor told you to take with a small sip of water. •Your doctor or nurse will tell you when to arrive at the hospital. What happens during a knee arthroscopy An arthroscopy can take from 15 minutes to over an hour, depending on how much work your surgeon needs to do inside your knee joint. Four different types of pain relief (anesthesia) may be used for knee arthroscopy surgery. Once the anaesthetic has taken effect, your surgeon will make small cuts in the skin around your knee joint. He or she will pump sterile fluid into your joint to help produce a clearer picture and then insert the arthroscope.
Your surgeon will examine your knee joint by looking at images sent by the arthroscope to a monitor. If necessary, he or she can insert instruments to repair damage or remove material that interferes with movement or causes pain in your knee. Afterwards, your surgeon will drain the fluid out and close the cuts with stitches or adhesive strips. Then he or she will wrap a dressing and a bandage around your knee. After the Procedure After the surgery, you will have an ace bandage on your knee over the dressing. Most people go home the same day they have surgery. Your doctor will give you an exercise program to follow. You may need pain relief to help with any discomfort as the anaesthetic wears off. You will need to arrange for someone to drive you home. You should try to have a friend or relative stay with you for the first 24 hours. Your nurse will give you some advice about caring for your healing wounds before you go home. You may be given a date for a follow-up appointment. The length of time your dissolvable stitches will take to disappear depends on what type you have. However, for this procedure they should usually disappear in about six weeks. Non-dissolvable stitches are removed 10 to 14 days after surgery. Recovery Recovery from knee arthroscopy is much faster than recovery from traditional open knee surgery. Still, it is important to follow your orthopaedic surgeon's instructions carefully after you return home. You should ask someone to check on you the first evening you are home. Some people may have to wear special pads, attached to an intermittent compression pump, on their lower legs. The pump inflates the pads and encourages healthy blood flow in your legs and helps to prevent DVT.
You may also be wearing compression stockings on your unaffected leg to help maintain circulation. You will have a dressing and an elasticated bandage over your knee joint. These apply pressure to assist with healing. You need to keep your knee clean and dry for about one to two weeks. You should use waterproof plasters over your healing wounds when you take a shower and don't soak your knee in the bath until the cuts are fully healed. Continue with the exercises recommended by your physiotherapist, as they will help to improve your knee movement and strength. Your knee joint is likely to feel sore and swollen for at least a week. This can last longer if you have arthritis. Try to keep your leg raised on a chair or footstool when you're resting. You should apply a cold compress such as ice or a bag of frozen peas, wrapped in a towel, to help reduce swelling and bruising. Don’t apply ice directly to your skin as it can damage your skin.
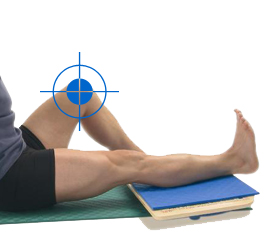
Follow your surgeon's advice about driving. You shouldn't drive until you're confident that you could perform an emergency stop without discomfort. This is usually about one to three weeks after your operation. Your recovery time will depend on what, if any, treatment your surgeon performs on your knee joint. You should be able to resume your usual activities after six to eight weeks depending on the severity of your knee problems and your level of fitness. Post –Operative Exercises and Physiotherapy Strengthening your thigh muscles (Quadriceps and Hamstrings) is most important. Swimming and cycling (stationary or road) are excellent ways to build these muscles up and improve movement.
Complications and Warning Signs As with any surgery, there are risks associated with knee arthroscopy. These occur infrequently and are minor and treatable. Complications Potential postoperative problems with knee arthroscopy include: •Infection •Blood clots •Accumulation of blood in the knee Warning Signs Call your orthopaedic surgeon immediately if you experience any of the following: •Fever •Chills •Persistent warmth or redness around the knee •Persistent or increased pain •Significant swelling in your knee •Increasing pain in your calf muscle Advantages of knee arthroscopy Unlike open surgery, arthroscopy results are expressed in less pain and stiffness, fewer complications, shorter hospital stay (if any) and faster recovery. For questions and additional information: Dr. Chanko Chankov tel: +359 2/960 49 50 www.orthopaedics.bg |




 Surgery performed in "VITA" Hospital
Surgery performed in "VITA" Hospital